Distinguishing between boils and cysts represents a fundamental challenge in dermatological assessment, yet understanding these differences proves crucial for appropriate treatment and patient outcomes. Both conditions manifest as localised skin lesions that can cause considerable discomfort and cosmetic concern, but their underlying pathophysiology, clinical presentation, and management approaches differ significantly. The ability to accurately differentiate between these two common skin conditions enables healthcare providers to implement targeted therapeutic interventions whilst reducing the risk of complications.
The prevalence of both boils and cysts in clinical practice underscores the importance of precise diagnostic skills. Research indicates that approximately 15% of the population will experience at least one significant skin cyst during their lifetime, whilst bacterial skin infections, including boils, account for over 2.3 million emergency department visits annually. These statistics highlight the substantial burden these conditions place on healthcare systems and emphasise the need for accurate initial assessment.
Clinical definition and pathophysiology of boils and cysts
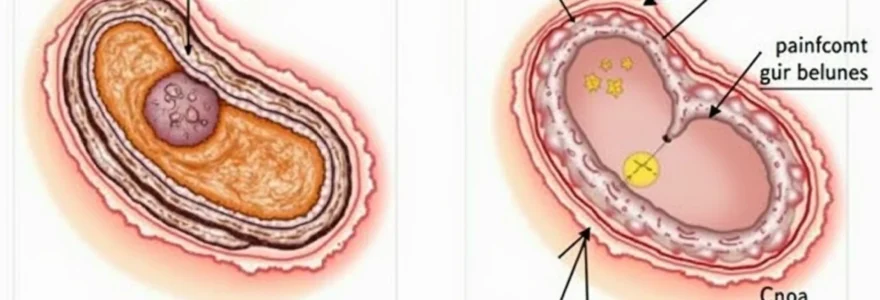
The fundamental distinction between boils and cysts lies in their underlying pathophysiological mechanisms and cellular origins. Understanding these processes provides the foundation for accurate diagnosis and appropriate therapeutic intervention. Each condition follows distinct developmental pathways that ultimately determine their clinical characteristics and treatment requirements.
Furuncle formation through staphylococcus aureus infection
A boil, medically termed a furuncle, develops through the invasion of hair follicles by pathogenic bacteria, predominantly Staphylococcus aureus . This gram-positive organism possesses numerous virulence factors that enable tissue invasion and destruction. The infection typically begins when bacteria breach the follicular epithelium through microscopic trauma or pre-existing skin compromise. Following bacterial inoculation, the host inflammatory response triggers neutrophil recruitment and activation, leading to pus formation and tissue necrosis.
The pathogenesis involves complex interactions between bacterial toxins and host immune responses. Staphylococcus aureus produces various enzymes, including hyaluronidase and coagulase, which facilitate tissue penetration and clot formation respectively. The resulting inflammatory cascade produces the characteristic clinical features of warmth, erythema, swelling, and pain that define boil presentations.
Sebaceous cyst development via keratin accumulation
Sebaceous cysts, more accurately termed epidermoid cysts, arise from the abnormal proliferation and retention of keratinocytes within enclosed epithelial-lined cavities. These benign lesions develop when the normal process of keratin shedding becomes disrupted, leading to progressive accumulation of proteinaceous material. The cyst wall consists of stratified squamous epithelium that continues to produce keratin, creating a self-perpetuating cycle of enlargement.
The biochemical composition of sebaceous cyst contents includes primarily keratin proteins, along with cholesterol crystals and cellular debris. This distinctive composition creates the characteristic cottage cheese-like appearance and often unpleasant odour associated with these lesions when ruptured. Unlike boils, sebaceous cysts lack the acute inflammatory component unless secondary bacterial infection occurs.
Epidermoid cyst pathogenesis and follicular occlusion
Epidermoid cysts represent another variant of keratin-containing lesions that develop through follicular occlusion mechanisms. These cysts form when hair follicle openings become blocked, preventing the normal extrusion of keratinaceous material. The trapped keratin accumulates within the follicular structure, gradually expanding to form a discrete cystic lesion. This process differs from sebaceous cyst formation in that it specifically involves pre-existing follicular anatomy.
The occlusion may result from various factors, including genetic predisposition, hormonal influences, or external trauma. Certain individuals demonstrate increased susceptibility to follicular occlusion, particularly those with conditions such as hidradenitis suppurativa or acne vulgaris. The resulting cysts typically maintain their connection to the original follicular structure, which may influence their clinical behaviour and recurrence patterns.
Pilonidal cyst aetiology in sacrococcygeal region
Pilonidal cysts represent a specialised form of cystic disease that develops specifically in the sacrococcygeal region through unique aetiological mechanisms. These lesions arise from the abnormal implantation of hair follicles into the subcutaneous tissues, often triggered by repetitive trauma or prolonged sitting. The term “pilonidal” literally means “nest of hair,” reflecting the characteristic finding of embedded hair shafts within these lesions.
The pathogenesis involves the creation of microscopic pits or sinuses in the natal cleft, which subsequently trap hair and debris. This trapped material acts as a foreign body, triggering chronic inflammatory responses and eventual cyst formation. The condition predominantly affects young adults, particularly males with excessive body hair, and those engaged in occupations requiring prolonged sitting.
Anatomical location patterns and distribution analysis
The anatomical distribution of boils and cysts follows predictable patterns that reflect their underlying pathophysiology and predisposing factors. Understanding these location preferences assists clinicians in developing differential diagnoses and guides appropriate investigation strategies. The relationship between lesion location and aetiology provides valuable diagnostic clues that complement physical examination findings.
Boil predilection sites: neck, axillae, and buttocks
Boils demonstrate a marked preference for areas characterised by high bacterial colonisation, increased moisture, and frequent friction. The neck region, particularly the posterior aspect, provides an ideal environment for Staphylococcus aureus proliferation due to its warm, moist conditions and regular contact with clothing collars. Studies indicate that cervical boils account for approximately 35% of all furuncle presentations, making this the most common anatomical site.
The axillary region represents another high-risk area due to its unique microenvironment. The combination of apocrine gland activity, hair follicle density, and mechanical friction creates optimal conditions for bacterial invasion. Axillary boils often present with more severe pain due to the rich innervation of this region and the involvement of deeper tissue planes. The buttocks, particularly the gluteal cleft, also demonstrates high susceptibility due to pressure-related trauma and bacterial seeding from the gastrointestinal tract.
Sebaceous cyst common locations: face, scalp, and trunk
Sebaceous cysts exhibit a distribution pattern that correlates closely with sebaceous gland density throughout the body. The face, particularly the central regions including the nose, cheeks, and forehead, represents the most common site for these lesions. This distribution reflects the high concentration of sebaceous glands in facial skin and their increased activity under hormonal influences. Facial sebaceous cysts often present unique management challenges due to cosmetic considerations and the risk of scarring.
The scalp serves as another frequent location for sebaceous cyst development, with these lesions often becoming quite large before detection due to concealment by hair. Scalp cysts may interfere with hair growth patterns and create significant cosmetic concerns. The trunk, including the chest and back regions, also demonstrates high susceptibility, particularly in areas prone to friction from clothing or repetitive mechanical trauma.
Ganglion cyst occurrence in wrist and hand joints
Ganglion cysts represent a distinct category of cystic lesions that develop in association with joint capsules and tendon sheaths. These lesions most commonly affect the wrist and hand, with the dorsal wrist accounting for approximately 60-70% of all ganglion cyst presentations. The pathogenesis involves the herniation of synovial fluid through joint capsule defects, creating fluid-filled sacs that maintain communication with the underlying joint space.
The clinical significance of ganglion cysts extends beyond cosmetic concerns, as they may interfere with joint function and cause mechanical symptoms. These lesions often fluctuate in size based on activity levels and joint position, a characteristic feature that aids in diagnosis. The proximity to important neurovascular structures in the hand and wrist requires careful assessment before therapeutic intervention.
Baker’s cyst formation behind knee joint
Baker’s cysts, also known as popliteal cysts, develop in the posterior aspect of the knee joint through the herniation of synovial fluid into the gastrocnemius-semimembranosus bursa. These lesions typically arise secondary to intra-articular pathology, such as meniscal tears or osteoarthritis, which increases synovial fluid production and pressure within the joint space. The resulting fluid accumulation creates a palpable mass in the popliteal fossa that may cause discomfort and functional limitation.
The clinical presentation of Baker’s cysts often includes symptoms of tightness or fullness behind the knee, particularly with knee flexion. These lesions may occasionally rupture, causing acute calf pain and swelling that can mimic deep vein thrombosis. The differential diagnosis of popliteal masses requires careful consideration of vascular pathology, including popliteal aneurysms and venous malformations.
Morphological characteristics and physical examination findings
The physical examination provides crucial diagnostic information for distinguishing between boils and cysts through systematic assessment of morphological characteristics. Each condition exhibits distinctive features that, when properly recognised, enable accurate diagnosis and appropriate treatment planning. The examination should encompass visual inspection, palpation, and assessment of associated signs and symptoms.
Boils typically present as erythematous, tender, fluctuant masses with surrounding induration and warmth. The lesions often demonstrate a central punctum or “head” containing purulent material, and the overlying skin may appear thinned or necrotic. Palpation reveals significant tenderness, and the lesion may feel warm compared to surrounding tissue. The presence of lymphadenopathy in the regional drainage area suggests more extensive bacterial involvement and potential systemic spread.
In contrast, cysts generally appear as well-circumscribed, mobile masses beneath the skin surface with normal overlying epidermis. The lesions typically feel firm or rubbery on palpation and demonstrate minimal tenderness unless secondary infection has occurred. Sebaceous cysts may exhibit a characteristic central punctum representing the original follicular opening, whilst other cyst types usually lack this feature. The absence of surrounding erythema and warmth helps distinguish uncomplicated cysts from infected lesions.
The assessment of lesion mobility provides valuable diagnostic information. Cysts typically demonstrate good mobility relative to underlying structures due to their encapsulated nature, whilst boils often feel fixed due to surrounding inflammatory changes. The presence of fluctuance indicates fluid content and may be observed in both conditions, though the quality of fluctuance differs. Boils exhibit a softer, more readily detectable fluctuance due to their purulent contents, whilst cysts may feel more tense due to their proteinaceous material.
Inflammatory response differences in acute presentations
The inflammatory response patterns associated with boils and cysts differ significantly in both local and systemic manifestations. These differences reflect the underlying pathophysiological mechanisms and provide important diagnostic clues during clinical assessment. Understanding these inflammatory patterns enables clinicians to gauge disease severity and select appropriate therapeutic interventions.
Boils generate intense acute inflammatory responses characterised by the classic signs of infection: dolor (pain), calor (heat), rubor (redness), tumor (swelling), and functio laesa (loss of function). The bacterial invasion triggers robust neutrophil recruitment and activation, leading to the release of inflammatory mediators such as interleukin-1β, tumour necrosis factor-α, and various chemokines. This inflammatory cascade produces the characteristic clinical features and may progress to systemic involvement with fever, malaise, and elevated white blood cell counts.
The severity of inflammatory response in boils correlates with bacterial virulence factors and host immune status. Methicillin-resistant Staphylococcus aureus (MRSA) infections often produce more severe inflammatory responses due to enhanced toxin production and antibiotic resistance. Patients with compromised immune systems, diabetes mellitus, or other predisposing conditions may exhibit altered inflammatory responses that complicate diagnosis and treatment.
Cysts typically demonstrate minimal inflammatory response unless secondary bacterial infection occurs. The encapsulated nature of most cysts prevents the release of antigenic material that would trigger significant immune responses. However, spontaneous cyst rupture can release keratin and other contents into surrounding tissues, producing a foreign body reaction characterised by granulomatous inflammation. This response, whilst intense, differs qualitatively from the neutrophilic inflammation seen in boils.
The key to distinguishing inflammatory responses lies in recognising that boils produce acute pyogenic inflammation, whilst cysts generate chronic granulomatous reactions only when their contents escape the capsule.
Diagnostic imaging techniques: ultrasound and MRI assessment
Advanced imaging modalities provide valuable supplementary information for differentiating boils and cysts, particularly in cases where clinical examination alone proves insufficient for definitive diagnosis. The selection of appropriate imaging techniques depends on lesion location, suspected pathology, and clinical complexity. Modern imaging approaches offer non-invasive methods for assessing internal structure, vascularity, and relationship to surrounding tissues.
High-frequency ultrasound for superficial lesion evaluation
High-frequency ultrasound (15-20 MHz) represents the imaging modality of choice for evaluating superficial skin lesions, providing excellent resolution of cutaneous and subcutaneous structures. This technique offers real-time assessment of lesion characteristics whilst remaining cost-effective and readily accessible. Ultrasound examination can differentiate solid from cystic lesions, assess vascularity through Doppler studies, and guide therapeutic interventions.
Boils typically demonstrate heterogeneous echogenicity with surrounding tissue oedema and increased vascularity on Doppler examination. The presence of fluid collections and tissue necrosis creates characteristic acoustic patterns that aid in diagnosis. Serial ultrasound examinations can monitor treatment response and identify complications such as abscess formation or deep tissue extension. The technique proves particularly valuable for assessing lesions in anatomically complex regions where clinical examination may be limited.
Cysts generally exhibit homogeneous hypoechoic or anechoic internal contents with well-defined walls and posterior acoustic enhancement. The uniform internal architecture reflects the proteinaceous nature of cyst contents and absence of inflammatory changes. Sebaceous cysts may demonstrate layered contents due to gravitational settling of debris, creating characteristic imaging appearances. The assessment of wall thickness and regularity helps predict the likelihood of successful conservative management versus surgical intervention.
T2-weighted MRI signal characteristics in cystic lesions
Magnetic resonance imaging provides superior soft tissue contrast and multiplanar assessment capabilities for complex cases requiring detailed anatomical evaluation. T2-weighted sequences prove particularly valuable for characterising cystic lesions due to their sensitivity to fluid content and tissue composition. The technique offers excellent delineation of lesion margins and relationship to critical structures such as blood vessels, nerves, and joint spaces.
Cysts typically demonstrate high T2 signal intensity reflecting their fluid content, with signal characteristics varying based on protein concentration and presence of debris. Simple cysts exhibit homogeneous high T2 signal, whilst complex cysts may show heterogeneous patterns due to proteinaceous content or haemorrhage. The presence of rim enhancement following gadolinium administration suggests inflammatory changes or infection. MRI proves especially valuable for deep-seated cysts and those located near critical anatomical structures.
Boils and abscesses demonstrate characteristic MRI appearances including central high T2 signal representing purulent content surrounded by rim enhancement and surrounding tissue oedema. The technique can identify complications such as deep tissue extension, osteomyelitis, or vascular involvement. Diffusion-weighted imaging may provide additional information regarding lesion cellularity and treatment response. The superior contrast resolution of MRI makes it invaluable for surgical planning in complex cases.
Doppler flow assessment for vascular involvement
Doppler ultrasound assessment provides crucial information regarding vascular involvement and perfusion patterns in skin lesions. This technique enables real-time evaluation of blood flow characteristics and can identify complications such as vessel compression or thrombosis. The assessment of vascularity also aids in determining lesion activity and predicting treatment response.
Boils typically demonstrate increased peripheral vascularity due to inflammatory hyperaemia, whilst the central region may show decreased flow due to tissue necrosis and thrombosis. Power Doppler techniques can detect low-velocity flow that may be missed by conventional colour Doppler. The pattern of vascular enhancement correlates with inflammatory activity and can guide timing of therapeutic interventions. Serial Doppler examinations help monitor treatment response and identify potential complications.
Treatment protocols and surgical management options
The therapeutic approach to boils an
d cysts requires careful consideration of multiple factors including lesion characteristics, patient factors, and potential complications. The selection of appropriate therapeutic modalities depends on accurate diagnosis, assessment of disease severity, and consideration of patient preferences. Modern treatment approaches emphasise evidence-based protocols that optimise outcomes whilst minimising morbidity and recurrence rates.The management strategy should account for the distinct pathophysiological differences between boils and cysts. Boils, being infectious processes, require antimicrobial therapy and drainage procedures, whilst cysts may be managed conservatively or through surgical excision. The timing of intervention plays a crucial role in treatment success, with early recognition and appropriate therapy preventing complications and reducing patient suffering.
Incision and drainage procedure for fluctuant boils
Incision and drainage represents the gold standard treatment for fluctuant boils, providing immediate symptomatic relief and facilitating bacterial clearance. The procedure should be performed under sterile conditions using appropriate local anaesthesia to ensure patient comfort and optimal surgical conditions. Current guidelines recommend culture of purulent material to guide antibiotic selection, particularly given the increasing prevalence of antimicrobial-resistant organisms.
The surgical technique involves creating an adequate incision through the most fluctuant portion of the lesion, allowing complete evacuation of purulent contents. The cavity should be irrigated with normal saline to remove residual debris and loculations broken down gently with a sterile instrument. Packing may be required for larger cavities to prevent premature closure and facilitate continued drainage. Post-operative care includes regular wound assessment, dressing changes, and patient education regarding signs of complications.
Complications of incision and drainage include incomplete drainage, recurrence, and spread of infection to surrounding tissues. The procedure should be avoided in cases of suspected deep tissue involvement or systemic toxicity, where more aggressive surgical intervention may be required. Follow-up examination within 48-72 hours ensures adequate healing and identifies potential complications requiring further intervention.
Complete excision technique for recurrent sebaceous cysts
Complete surgical excision represents the definitive treatment for sebaceous cysts, offering the lowest recurrence rates when performed correctly. The technique requires careful dissection of the entire cyst wall to prevent incomplete removal and subsequent recurrence. Pre-operative planning should include assessment of cyst location, size, and relationship to vital structures to ensure optimal surgical approach and cosmetic outcomes.
The surgical procedure begins with adequate local anaesthetic infiltration, taking care to avoid injection directly into the cyst cavity which may cause rupture and complicate dissection. An elliptical incision incorporating the central punctum, if present, allows complete removal whilst minimising tissue trauma. Meticulous dissection along the cyst wall plane preserves surrounding tissues and facilitates primary closure. Intact cyst removal prevents spillage of contents and reduces inflammatory complications.
Post-operative care includes appropriate wound closure techniques, with subcuticular sutures preferred for optimal cosmetic results in visible areas. Patients should receive clear instructions regarding wound care, activity restrictions, and signs requiring medical attention. Histopathological examination of excised specimens confirms diagnosis and excludes malignancy, though this remains extremely rare in typical sebaceous cysts.
Antibiotic therapy: flucloxacillin and clindamycin selection
Antibiotic selection for boil treatment should be guided by local resistance patterns and culture results when available. Flucloxacillin remains the first-line oral antibiotic for uncomplicated staphylococcal skin infections, providing excellent coverage against methicillin-sensitive Staphylococcus aureus. The typical dosing regimen involves 500mg four times daily for 7-10 days, with dose adjustments required for renal impairment or hepatic dysfunction.
Clindamycin serves as an excellent alternative for patients with penicillin allergies or suspected MRSA infections. This agent demonstrates good tissue penetration and maintains activity against many resistant staphylococcal strains. The standard oral dose is 300-450mg four times daily, with careful monitoring for gastrointestinal side effects including Clostridium difficile-associated diarrhoea. Duration of therapy should be individualised based on clinical response and severity of infection.
Empirical antibiotic therapy may be initiated pending culture results in patients with severe infections, systemic symptoms, or high-risk features. Intravenous antibiotics should be considered for patients with extensive cellulitis, bacteraemia, or failure to respond to oral therapy. Regular reassessment ensures appropriate modification of antimicrobial regimens based on clinical response and microbiological results.
Intralesional corticosteroid injection for inflamed cysts
Intralesional corticosteroid injection offers an effective treatment option for inflamed cysts that have not responded to conservative management. This technique can provide rapid symptom relief and may facilitate resolution without surgical intervention. Triamcinolone acetonide remains the most commonly used agent, typically administered at concentrations of 10-40mg/ml depending on lesion size and location.
The injection technique requires careful needle placement into the cyst cavity, avoiding injection into surrounding normal tissue which may cause local atrophy. Multiple injection sites may be necessary for larger lesions, with total corticosteroid dose calculated based on lesion volume and patient factors. Post-injection massage helps distribute the medication throughout the cyst cavity and may enhance therapeutic efficacy.
Potential complications include skin atrophy, depigmentation, and temporary worsening of inflammation. These risks can be minimised through appropriate patient selection, correct injection technique, and use of appropriate corticosteroid concentrations. Follow-up assessment at 2-4 weeks allows evaluation of treatment response and planning of additional interventions if necessary. Patients should be counselled regarding expected outcomes and potential need for alternative treatments if intralesional injection proves ineffective.