Nail bed injuries represent some of the most common yet challenging trauma cases encountered in clinical practice, affecting millions of individuals annually through accidents, sports injuries, and occupational hazards. The human nail bed possesses remarkable regenerative capabilities that have fascinated medical professionals for decades, yet the extent and mechanisms of this regeneration remain subjects of ongoing research and clinical investigation. Understanding whether and how the nail bed can regrow after injury has profound implications for treatment decisions, surgical interventions, and long-term patient outcomes. The intricate interplay between cellular biology, vascular supply, and mechanical factors determines the success of nail bed regeneration, making this topic crucial for healthcare providers treating digital trauma.
Nail bed anatomy and cellular regeneration mechanisms
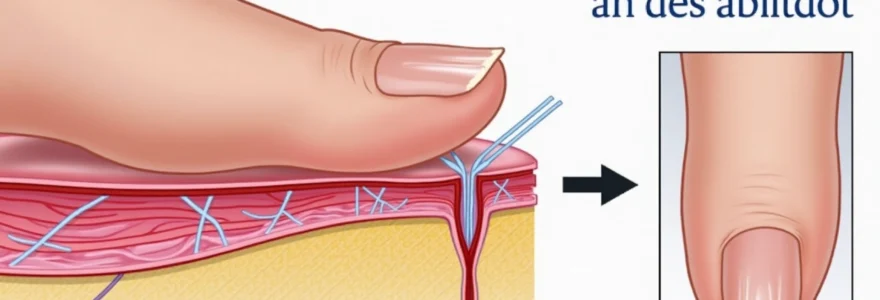
The nail bed represents a highly specialised anatomical structure designed to support continuous nail growth throughout human life. This complex tissue comprises multiple layers, each serving distinct physiological functions that contribute to the overall regenerative capacity of the nail apparatus. The nail bed extends from the lunula proximally to the hyponychium distally, creating a foundation upon which the nail plate adheres and grows.
Germinal matrix structure and keratinocyte production
The germinal matrix serves as the primary engine of nail production, containing highly active keratinocyte stem cells that divide continuously to generate new nail tissue. Research indicates that approximately 90% of nail growth originates from this critical region, which lies beneath the proximal nail fold. These specialised cells undergo rapid mitosis, producing layers of keratinised cells that eventually form the hard nail plate. The sterile matrix, located more distally, contributes the remaining 10% of nail growth whilst playing a crucial role in nail plate adhesion to the underlying bed.
Cellular regeneration within the germinal matrix follows a precise pattern of stem cell activation, proliferation, and differentiation. When injury occurs, dormant stem cell populations become activated through various growth factor signals, initiating the repair process. The matrix produces approximately 196 distinct cellular layers that combine to form each complete nail structure, demonstrating the remarkable complexity of this regenerative system.
Vascular supply through digital arteries and capillary networks
The nail bed receives its blood supply through an intricate network of digital arteries that branch into numerous capillary beds throughout the tissue. This rich vascular architecture plays a fundamental role in supporting the high metabolic demands of continuously dividing cells within the matrix regions. The arterial supply includes contributions from both palmar and dorsal digital arteries, creating redundant circulation pathways that help maintain tissue viability during injury.
Microvascular density within the nail bed exceeds that found in many other body tissues, reflecting the intensive cellular activity required for continuous nail production. Following trauma, this vascular network must rapidly reorganise to deliver essential nutrients and oxygen to regenerating tissues. Angiogenesis , the formation of new blood vessels, becomes particularly important during the healing phase, as damaged vessels require replacement to support tissue regeneration.
Neural innervation and sensory receptor distribution
The nail bed contains an extensive network of sensory nerve endings that provide tactile feedback and pain sensation. These neural structures include mechanoreceptors, nociceptors, and thermoreceptors distributed throughout the tissue layers. The high density of nerve endings explains why nail bed injuries typically produce intense pain sensations that can persist throughout the healing process.
Neural regeneration following nail bed injury occurs through axonal sprouting and Schwann cell proliferation. This process can take several months to complete, during which patients may experience altered sensation in the affected digit. The restoration of proper innervation proves essential for normal nail bed function and the return of protective sensory feedback.
Extracellular matrix composition and collagen framework
The extracellular matrix (ECM) of the nail bed consists primarily of type I and type III collagen fibres , providing structural support for cellular components and maintaining tissue architecture. This framework includes elastin fibres, proteoglycans, and various glycoproteins that facilitate cell migration and adhesion during regeneration. The ECM serves as a scaffold upon which new tissue can grow following injury.
During the healing process, fibroblasts within the nail bed produce new collagen and other matrix components to replace damaged structures. The quality and organisation of this newly formed matrix significantly influences the final appearance and function of the regenerated nail bed. Proper matrix remodelling requires several months to achieve optimal strength and flexibility.
Classification of nail bed injuries and tissue damage assessment
Understanding the various types of nail bed injuries provides essential context for evaluating regenerative potential and determining appropriate treatment strategies. Medical professionals utilise standardised classification systems to assess injury severity and predict healing outcomes. The extent of tissue damage directly correlates with the likelihood of successful regeneration and the complexity of required interventions.
Subungual haematoma and blood accumulation patterns
Subungual haematomas develop when blood vessels beneath the nail plate rupture, typically following crush injuries or direct trauma to the digit. The accumulation of blood creates characteristic dark discolouration visible through the nail plate, accompanied by intense throbbing pain due to pressure buildup in the confined space. The size and location of the haematoma provide important prognostic indicators for nail bed recovery.
Haematomas covering less than 25% of the nail bed generally resolve without intervention, allowing normal regeneration to occur. However, larger accumulations may indicate more extensive underlying tissue damage requiring medical evaluation. The presence of blood can also create favourable conditions for bacterial growth, potentially complicating the healing process if proper care is not provided.
Laceration severity using zook classification system
The Zook classification system provides a standardised approach to categorising nail bed lacerations based on the structures involved and the complexity of repair required. Simple lacerations involve only the nail bed, whilst complex injuries may include damage to the nail matrix, surrounding soft tissues, or underlying bone. This classification helps guide treatment decisions and predict functional outcomes.
Linear lacerations parallel to the nail growth direction typically heal more favourably than perpendicular cuts, which can disrupt the normal architecture of the nail bed. Stellate or crush-type lacerations present greater challenges for repair due to tissue loss and irregular wound margins. The involvement of the germinal matrix in any laceration significantly impacts the potential for normal nail regrowth.
Crush injuries and cellular necrosis evaluation
Crush injuries to the nail bed result from compression forces that damage cellular structures and disrupt vascular supply. These injuries often produce zones of tissue necrosis where cells cannot survive due to inadequate blood flow or direct cellular damage. The extent of necrotic tissue determines the regenerative capacity of the remaining viable nail bed.
Assessment of tissue viability following crush injury requires careful examination of capillary refill, tissue colour, and bleeding patterns. Areas of tissue that appear white or grey typically indicate compromised circulation and reduced regenerative potential. The presence of extensive necrosis may necessitate surgical debridement to remove non-viable tissue and promote healing of healthy structures.
Avulsion trauma and eponychial fold disruption
Nail bed avulsions involve the separation of nail tissue from the underlying bed, either partially or completely. These injuries commonly occur when the nail becomes caught in machinery or during sudden pulling forces applied to the digit. Complete avulsions remove the protective nail plate and expose the sensitive nail bed to environmental trauma and infection risk.
Avulsion injuries frequently involve damage to the eponychial fold and surrounding soft tissues, complicating the repair process. The loss of these supporting structures can affect the final cosmetic appearance of the regenerated nail and may require specialised surgical techniques to restore normal anatomy. Early intervention proves crucial for optimising outcomes following avulsion trauma.
Physiological nail bed regeneration process and timeline
The regeneration of nail bed tissue following injury represents a complex biological process involving multiple phases of healing and cellular reorganisation. Understanding this timeline helps clinicians and patients establish realistic expectations for recovery and identify potential complications early in the healing process. The regenerative capacity of nail bed tissue varies significantly based on the extent of injury and individual patient factors.
Initial healing begins within hours of injury as inflammatory cascades activate cellular repair mechanisms. Haemostasis occurs first, with platelet aggregation and clot formation to control bleeding and create a stable foundation for subsequent healing phases. Within 24-48 hours, inflammatory cells migrate to the injury site, releasing cytokines and growth factors that stimulate cellular proliferation and tissue repair.
The proliferative phase commences approximately 3-5 days post-injury, characterised by rapid fibroblast migration and collagen synthesis. During this period, new blood vessels begin forming through angiogenesis, re-establishing circulation to damaged areas. Epithelialisation of the nail bed surface typically begins within the first week, with cells migrating from wound edges to cover exposed areas.
Nail matrix regeneration follows a more prolonged timeline, often requiring 4-6 weeks for basic structural restoration. However, complete functional recovery may take 6-9 months as new nail growth must occur to replace the damaged nail plate.
The nail bed demonstrates remarkable regenerative capacity when the germinal matrix remains intact, often achieving near-normal function within six months of injury.
Remodelling represents the final phase of nail bed regeneration, continuing for up to 12-18 months post-injury. During this extended period, newly formed collagen fibres reorganise to restore optimal tissue strength and flexibility. The final appearance and function of the regenerated nail bed depends largely on the success of this remodelling phase and the prevention of complications such as adhesion formation or infection.
Clinical factors affecting nail bed regrowth potential
Multiple clinical variables influence the success of nail bed regeneration, ranging from patient-specific characteristics to environmental factors that affect healing. Recognition of these variables allows healthcare providers to optimise treatment approaches and counsel patients regarding expected outcomes. The interplay between these factors often determines whether regeneration proceeds normally or encounters significant obstacles.
Patient age and cellular proliferation capacity
Age represents one of the most significant factors affecting nail bed regeneration, with younger patients generally demonstrating superior healing capacity compared to older individuals. Paediatric patients exhibit enhanced cellular proliferation rates and more robust angiogenic responses, leading to faster and more complete tissue regeneration. The regenerative potential gradually declines with advancing age due to reduced stem cell activity and decreased metabolic efficiency.
Children typically achieve complete nail bed regeneration within 3-4 months following injury, whilst elderly patients may require 6-12 months for comparable healing. The quality of regenerated tissue also varies by age, with younger patients more likely to achieve normal nail appearance and function. Cellular senescence in older adults can limit the extent of regeneration and increase the risk of complications such as chronic pain or nail deformity.
Infection risk and staphylococcus aureus complications
Bacterial infection poses a significant threat to successful nail bed regeneration, with Staphylococcus aureus representing the most common pathogenic organism encountered in digital trauma. The warm, moist environment created by bandages and the presence of devitalised tissue provide ideal conditions for bacterial proliferation. Infection can rapidly destroy regenerating tissue and lead to permanent functional impairment.
Prevention of infection requires meticulous wound care, appropriate antibiotic prophylaxis when indicated, and regular monitoring for signs of complications. Early recognition of infection allows for prompt intervention that can preserve regenerative potential. Chronic infection may necessitate surgical debridement or other aggressive interventions that can compromise the final outcome.
Diabetes mellitus impact on microvascular healing
Patients with diabetes mellitus face unique challenges in nail bed regeneration due to compromised microvascular function and impaired cellular metabolism. Chronic hyperglycaemia damages small blood vessels throughout the body, reducing oxygen and nutrient delivery to healing tissues. This microvascular insufficiency significantly slows the regeneration process and increases the risk of complications.
Diabetic patients require enhanced monitoring and may benefit from advanced wound care technologies to optimise healing conditions. Blood glucose control becomes paramount during the recovery period, as persistent hyperglycaemia can halt regeneration entirely. The risk of infection also increases substantially in diabetic individuals, necessitating aggressive preventive measures.
Immunosuppression and delayed epithelialisation
Immunocompromised patients, whether due to medication effects or underlying disease processes, demonstrate impaired nail bed regeneration capacity. The immune system plays crucial roles in wound healing, including debris clearance, growth factor production, and infection prevention. Immunosuppression disrupts these processes, leading to delayed healing and increased complication rates.
Patients receiving chemotherapy, organ transplant recipients, or individuals with autoimmune disorders require specialised care approaches during nail bed recovery. Close collaboration between multiple specialists may be necessary to balance immunosuppressive therapy needs with healing requirements. Alternative treatment strategies, including biological dressings or growth factor supplementation, may prove beneficial in these challenging cases.
Advanced surgical techniques for nail bed reconstruction
When natural regeneration proves insufficient or impossible due to extensive tissue loss, surgical reconstruction techniques can restore functional nail bed anatomy. These advanced procedures require specialised expertise and careful patient selection to achieve optimal outcomes. The choice of reconstructive technique depends on the extent of tissue damage, patient factors, and the desired functional and cosmetic results.
Split-thickness skin grafting from hypothenar eminence
Split-thickness skin grafting represents a well-established technique for reconstructing large nail bed defects when primary closure is not possible. The hypothenar eminence provides an ideal donor site due to its similar tissue characteristics and relatively inconspicuous scarring. This technique allows coverage of exposed bone or tendon whilst providing a foundation for potential nail regrowth.
Successful grafting requires meticulous preparation of the recipient bed to ensure adequate vascularity for graft survival. The harvested graft must be carefully secured and protected during the initial healing period to prevent shearing forces that could compromise integration. Graft take typically occurs within 5-7 days, with complete healing achieved in 3-4 weeks. However, the cosmetic result may differ from normal nail bed appearance, and nail regrowth over the grafted area often exhibits irregular characteristics.
Germinal matrix transplantation using zook protocol
The Zook protocol for germinal matrix transplantation offers the potential for true nail bed regeneration when the native matrix is severely damaged or destroyed. This technique involves harvesting viable matrix tissue from an uninjured digit and transplanting it to the damaged area. The procedure requires microsurgical precision to maintain cellular viability and achieve proper positioning of the transplanted tissue.
Success rates for matrix transplantation vary depending on the extent of injury and surgical expertise, with reports ranging from 60-85% for achieving functional nail regrowth. The transplanted matrix requires several months to establish adequate blood supply and begin producing new nail tissue.
Germinal matrix transplantation represents the gold standard for restoration of nail growth when native structures cannot be preserved, though success depends heavily on surgical technique and post-operative care.
Microsurgical anastomosis for vascular restoration
Complex nail bed injuries may require microsurgical vascular repair to restore adequate circulation for tissue survival and regeneration. This technique involves the precise reconnection of severed blood vessels using magnification and specialised instruments. Successful vascular repair can mean the difference between tissue survival and necrosis in severe crush or avulsion injuries.
The technical demands of microsurgical anastomosis require extensive training and experience to achieve consistent results. Even small errors in technique can lead to vessel thrombosis and tissue loss. When successful, however, vascular repair enables natural regeneration processes to proceed and often produces superior long-term outcomes compared to alternative reconstructive methods.
Dermal substitute integration and biomatrix applications
Modern regenerative medicine offers innovative solutions for nail bed reconstruction through the use of dermal substitutes and bioengineered matrices. These materials provide scaffolding for cellular ingrowth whilst gradually being replaced by native tissue during the healing process. Collagen-based matrices and synthetic polymers have shown promising results in clinical applications.
The integration of dermal substitutes requires careful attention to wound preparation and post-operative management to optimise cellular infiltration and tissue remodelling. These materials can be particularly valuable when traditional grafting techniques are not suitable due to poor recipient site conditions or patient factors. Long-term studies continue to evaluate the durability and functional outcomes of these advanced reconstructive approaches.
Post-injury prognosis and Long-Term functional outcomes
The long-term prognosis following nail
bed injury remains largely favorable when appropriate treatment is implemented promptly and complications are avoided. The majority of patients can expect significant functional recovery within 6-12 months, though complete healing may extend beyond this timeframe in complex cases. Understanding the factors that influence long-term outcomes helps clinicians provide accurate prognostic information and guide treatment decisions throughout the recovery process.
Functional outcomes depend heavily on the preservation of the germinal matrix during initial injury and subsequent treatment. When this critical structure remains intact, nail regrowth rates approach 85-95% for achieving cosmetically acceptable results. However, matrix damage or loss significantly reduces the likelihood of normal nail appearance and function, often necessitating reconstructive procedures or prosthetic solutions.
The timeline for nail regrowth varies considerably based on injury location, with fingernails typically requiring 4-6 months for complete replacement whilst toenails may take 12-18 months. During this period, patients often experience gradual improvement in pain levels, sensitivity, and overall function. The newly formed nail may initially appear thicker, ridged, or discoloured, but these characteristics often improve with time as the nail bed remodels.
Long-term complications can significantly impact functional outcomes and quality of life for affected individuals. Chronic pain syndromes develop in approximately 15-20% of severe nail bed injuries, particularly those involving extensive soft tissue damage or bone involvement. Cold intolerance represents another common sequela, affecting up to 30% of patients and potentially persisting for several years following injury.
Research indicates that patients who receive prompt, appropriate treatment for nail bed injuries achieve functional outcomes comparable to the uninjured digit in approximately 80% of cases, emphasising the importance of early intervention.
Cosmetic concerns frequently persist even after successful functional recovery, with nail discolouration, irregular growth patterns, or permanent ridging affecting patient satisfaction with treatment outcomes. The psychological impact of these cosmetic changes should not be underestimated, as many patients report self-consciousness about their appearance and modifications to daily activities or occupational tasks.
Return to full activity levels depends on the nature of the patient’s occupation and recreational pursuits. Office workers typically resume normal activities within 4-6 weeks, whilst manual labourers or athletes may require 3-6 months before returning to pre-injury performance levels. The development of protective callusing and adaptation to altered sensation patterns contributes to functional improvement over time.
Factors predictive of superior long-term outcomes include younger patient age, absence of comorbid medical conditions, prompt initial treatment, and compliance with post-operative care instructions. Conversely, delayed treatment, infection, or inadequate immobilisation during healing correlate with poorer functional results and increased complication rates.
Follow-up care remains essential for monitoring regeneration progress and identifying potential complications early in their development. Regular assessments allow for timely intervention when healing deviates from expected patterns, potentially preventing permanent functional impairment. Patient education regarding realistic expectations and the prolonged nature of nail bed recovery helps maintain compliance with treatment protocols and reduces anxiety about the healing process.
The regenerative capacity of nail bed tissue represents one of the most remarkable examples of adult tissue repair in the human body. While complete restoration to pre-injury state may not always be achievable, the potential for meaningful functional recovery remains excellent in most cases when evidence-based treatment approaches are employed. Continued advances in reconstructive techniques and regenerative medicine offer hope for even better outcomes in the future, potentially transforming the prognosis for patients with severe nail bed injuries.