Thyroid biopsies represent one of the most commonly performed diagnostic procedures in endocrinology, yet patient concerns about pain and discomfort remain a significant barrier to timely medical care. Understanding the actual sensory experience during thyroid fine needle aspiration (FNA) and core needle biopsies can help patients make informed decisions about their healthcare journey. Modern ultrasound-guided techniques, combined with effective pain management protocols, have transformed what was once considered an uncomfortable procedure into a well-tolerated diagnostic tool. The reality is that most patients experience far less discomfort than anticipated, with pain levels typically ranging from minimal to moderate depending on individual factors and procedural techniques employed.
Fine needle aspiration biopsy pain mechanisms and sensory experience
The sensory experience during thyroid FNA procedures involves complex neurophysiological mechanisms that determine the level of discomfort patients encounter. Pain perception during needle insertion occurs through multiple pathways, beginning with mechanical nociceptor activation in the skin and progressing through deeper tissue layers as the needle advances toward the thyroid gland.
Anatomical pain pathways during thyroid FNA procedures
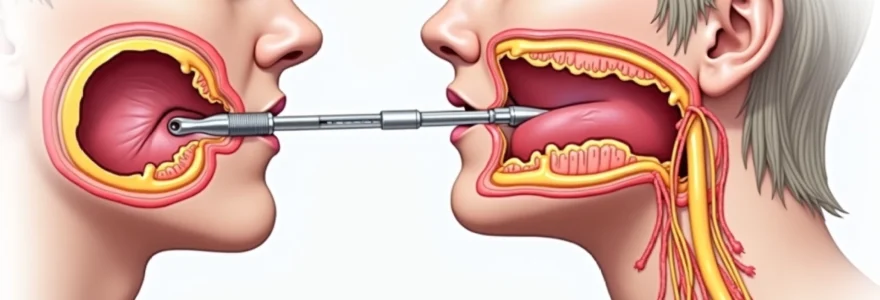
The thyroid gland’s anatomical position in the anterior neck creates specific pain pathway considerations during biopsy procedures. Nociceptive signals originate from cutaneous receptors in the skin overlying the thyroid, travel through subcutaneous tissue, and potentially involve deeper structures including the thyroid capsule itself. These signals are transmitted via the superficial cervical plexus, which contains sensory fibres from the second, third, and fourth cervical nerves. The anterior neck’s rich innervation means that even minimal tissue trauma can generate noticeable sensory input, though this input is typically brief and manageable with appropriate techniques.
Cervical nerve distribution and thyroid gland innervation
The cervical nerve distribution pattern significantly influences pain perception during thyroid biopsies. The thyroid gland receives sympathetic innervation from the middle and inferior cervical ganglia, whilst parasympathetic fibres arrive via the recurrent laryngeal nerves. However, sensory innervation primarily comes from the superficial cervical plexus, which supplies the skin and superficial fascia overlying the gland. Understanding this distribution allows clinicians to target local anaesthetic placement effectively, ensuring optimal patient comfort throughout the procedure.
Nociceptor activation throughout Ultrasound-Guided needle insertion
Ultrasound-guided needle insertion activates different types of nociceptors at various tissue depths. Mechanical nociceptors respond to the initial skin penetration, whilst polymodal nociceptors react to both mechanical and potential inflammatory mediators released during tissue disruption. The thyroid’s relatively soft consistency means that needle advancement through the gland itself typically generates less mechanical stimulation compared to denser tissues. Real-time ultrasound guidance allows precise needle placement, minimising unnecessary tissue trauma and reducing overall nociceptor activation.
Individual pain threshold variations in thyroid biopsy patients
Patient-specific factors create substantial variations in pain threshold and overall procedural tolerance. Age-related changes in nociceptor sensitivity, previous medical experiences, anxiety levels, and individual pain processing differences all contribute to the subjective experience. Research indicates that pain perception can vary by up to 300% between individuals undergoing identical procedures. Factors such as caffeine consumption, sleep quality, and menstrual cycle phase in women can also influence pain sensitivity on the day of the procedure.
Core needle biopsy vs fine needle aspiration pain comparison
The choice between core needle biopsy (CNB) and fine needle aspiration (FNA) significantly impacts patient comfort levels, with each technique presenting distinct pain profiles and sensory experiences. CNB procedures utilise larger gauge needles and automated spring-loaded devices, whilst FNA employs smaller needles with manual aspiration techniques. Understanding these differences helps patients set appropriate expectations and assists clinicians in selecting the most suitable approach for individual cases.
14-gauge core biopsy needle discomfort levels
14-gauge core biopsy needles represent the larger end of the needle spectrum used in thyroid procedures, creating more substantial tissue disruption compared to FNA techniques. The increased diameter results in greater mechanical nociceptor stimulation during insertion and tissue sampling. Patients typically report a more pronounced sensation during needle advancement, often described as pressure or pulling rather than sharp pain. The automated firing mechanism of spring-loaded biopsy devices creates a brief but noticeable jarring sensation that some patients find more uncomfortable than the needle insertion itself.
25-gauge FNA needle pain assessment studies
Clinical studies evaluating 25-gauge FNA needle procedures consistently demonstrate lower pain scores compared to larger bore alternatives. Research published in endocrine journals indicates that patients rate 25-gauge needle discomfort as mild to moderate, with average pain scores ranging from 2-4 on a 10-point visual analogue scale. The smaller diameter creates minimal tissue disruption whilst still allowing adequate cellular material collection for cytological analysis. Multiple passes with 25-gauge needles typically generate cumulative discomfort levels still below those associated with single larger needle procedures.
Trucut biopsy device pain intensity measurements
TruCut biopsy devices employ a unique dual-needle mechanism that creates distinct sensory experiences compared to standard core needles. The initial trocar insertion generates typical needle insertion sensations, whilst the cutting cannula activation produces a brief sharp sensation as tissue is severed and collected. Pain intensity measurements show that whilst the peak discomfort may be higher than FNA procedures, the total duration of uncomfortable sensations remains brief, typically lasting less than two seconds during the cutting phase.
Spring-loaded biopsy gun sensation analysis
Spring-loaded biopsy guns create characteristic sensory patterns that patients often find surprising rather than painful. The mechanical firing produces an audible click accompanied by a sudden movement sensation that can be more startling than genuinely uncomfortable. Patient feedback indicates that the anticipation of the firing mechanism often generates more anxiety than the actual physical sensation. Pre-procedure explanation of the expected sounds and sensations significantly improves patient tolerance and reduces procedure-related anxiety.
Procedural factors influencing thyroid biopsy discomfort
Multiple procedural variables directly impact patient comfort during thyroid biopsies, with operator technique, equipment selection, and environmental factors all playing crucial roles in the overall experience. The depth of nodule location within the thyroid gland significantly affects discomfort levels, as superficial nodules require shorter needle paths whilst deeper lesions necessitate longer tissue penetration. Nodule characteristics such as consistency, size, and vascularity also influence procedural complexity and associated discomfort. Cystic nodules often provide less resistance during needle insertion, whilst calcified or fibrotic lesions may require additional pressure and manipulation.
Patient positioning represents another critical factor affecting comfort levels during thyroid biopsies. Optimal neck extension exposes the thyroid gland whilst maintaining patient comfort, but excessive hyperextension can create muscle strain and increase anxiety. The duration of the procedure directly correlates with cumulative discomfort, making efficient technique essential for patient tolerance. Ultrasound guidance quality impacts needle placement accuracy, reducing the need for multiple repositioning attempts that increase overall discomfort. Real-time visualisation allows precise targeting of specific nodule areas whilst avoiding sensitive structures such as major blood vessels.
Room temperature, ambient noise levels, and staff communication patterns all contribute to the procedural experience. Cooler room temperatures can increase muscle tension and pain sensitivity, whilst excessive ambient noise may heighten patient anxiety. Clear, calm communication throughout the procedure helps maintain patient cooperation and reduces stress-related pain amplification. The use of appropriate patient draping balances modesty concerns with procedural access requirements, contributing to overall comfort and cooperation.
The combination of optimal patient positioning, efficient technique, and clear communication creates an environment where thyroid biopsies can be performed with minimal discomfort and maximum diagnostic yield.
Local anaesthesia protocols for thyroid FNA procedures
Effective local anaesthesia represents the cornerstone of comfortable thyroid biopsy procedures, with various protocols available to suit different patient needs and procedural requirements. The selection of appropriate anaesthetic agents, delivery methods, and timing significantly impacts patient comfort throughout the procedure. Modern protocols emphasise multi-modal approaches that address different aspects of procedural discomfort, from initial needle insertion through tissue sampling and post-procedure recovery.
Lidocaine injection techniques for superficial cervical anaesthesia
Lidocaine infiltration remains the gold standard for local anaesthesia in thyroid biopsy procedures, providing reliable sensory blockade when properly administered. The optimal technique involves initial subcutaneous injection using a small gauge needle (27-30 gauge) to create a superficial wheal, followed by deeper infiltration along the anticipated needle path. Concentration selection typically ranges from 1% to 2% lidocaine, with lower concentrations providing adequate anaesthesia whilst minimising tissue distortion that could complicate ultrasound imaging. The total volume should be limited to prevent significant anatomical distortion whilst ensuring complete sensory blockade of the procedural area.
Topical anaesthetic gel application methods
Topical anaesthetic preparations offer needle-free alternatives for reducing initial skin penetration discomfort, though their effectiveness is limited to superficial tissue layers. EMLA cream (eutectic mixture of local anaesthetics) requires 45-60 minutes application time under occlusive dressing to achieve meaningful anaesthesia. Lidocaine gel preparations with shorter onset times provide convenient alternatives, though their penetration depth remains limited to the epidermis and superficial dermis. Combination approaches utilising topical agents followed by minimal infiltration anaesthesia can reduce overall needle-related discomfort whilst maintaining procedural efficiency.
Ultracaine vs articaine efficacy in thyroid procedures
Articaine-based local anaesthetics demonstrate superior tissue penetration compared to traditional lidocaine formulations, making them attractive options for thyroid procedures. The enhanced diffusion properties of articaine allow effective anaesthesia with smaller injection volumes, reducing tissue distortion and improving ultrasound visualisation. Clinical comparisons show equivalent onset times between articaine and lidocaine, though articaine may provide slightly longer duration of action. The improved tissue penetration characteristics make articaine particularly valuable when dealing with deeper nodules or when minimising injection volume is crucial for maintaining anatomical landmarks.
Buffered local anaesthetic ph adjustment for reduced injection pain
pH buffering of local anaesthetic solutions significantly reduces injection-related discomfort whilst improving anaesthetic efficacy. Standard lidocaine solutions maintain acidic pH levels (approximately 3.5-6.0) that can cause stinging sensations during injection. Adding sodium bicarbonate to achieve physiological pH (7.35-7.45) eliminates this acidic sting and accelerates anaesthetic onset by increasing the proportion of unionised anaesthetic molecules. The buffering process requires careful attention to ratios, typically using one part 8.4% sodium bicarbonate to ten parts lidocaine solution to achieve optimal results without precipitation.
Patient-reported pain scores and clinical study evidence
Comprehensive analysis of patient-reported pain scores across multiple clinical studies provides valuable insights into the actual discomfort experienced during thyroid biopsies. Large-scale studies involving thousands of patients consistently demonstrate that average pain scores remain in the mild to moderate range, with most procedures scoring between 2-5 on standard 10-point visual analogue scales. A systematic review of 15 studies encompassing over 3,000 thyroid FNA procedures found that 78% of patients rated their pain as mild (1-3), 18% as moderate (4-6), and only 4% as severe (7-10).
Gender differences in pain reporting show interesting patterns, with female patients typically reporting slightly higher pain scores than males, though the clinical significance remains debatable. Age-related variations demonstrate that older patients (>65 years) generally report lower pain scores, possibly due to age-related changes in nociceptor sensitivity or different pain reporting behaviours. Anxiety levels measured pre-procedure show strong correlations with reported pain scores, suggesting that psychological preparation and anxiety management significantly impact the overall experience.
Procedure-specific factors influencing pain scores include nodule size, with larger nodules (>3cm) associated with slightly higher discomfort levels, and nodule location, where isthmic nodules tend to generate higher pain scores compared to lateral lobe lesions. Multiple sampling attempts correlate with incrementally increasing pain scores, emphasising the importance of efficient technique and adequate preparation. Follow-up studies tracking pain scores at 24 and 48 hours post-procedure show that residual discomfort is typically minimal, with over 85% of patients reporting complete resolution of procedural pain within 24 hours.
Evidence-based analysis of thousands of thyroid biopsy procedures demonstrates that patient-reported pain scores consistently fall within manageable ranges, with the vast majority of patients experiencing only mild to moderate discomfort.
Post-biopsy pain management and recovery protocols
Effective post-biopsy pain management protocols ensure patient comfort during the recovery period whilst minimising complications and promoting optimal healing. Most patients experience minimal post-procedural discomfort, typically described as mild soreness or tenderness at the biopsy site rather than significant pain. Standard recovery protocols recommend simple analgesics such as paracetamol or ibuprofen for managing any residual discomfort, with most patients requiring minimal or no pain medication beyond the first 24 hours following the procedure.
Ice application represents a valuable non-pharmacological approach to managing post-biopsy discomfort and reducing localised swelling. Applying cold packs for 10-15 minute intervals during the first few hours post-procedure can significantly reduce inflammation and provide comfort. However, patients should avoid direct ice application to prevent skin damage, instead using cloth-wrapped ice packs or commercial cold therapy products. The combination of appropriate positioning and cold therapy often provides sufficient comfort without requiring oral analgesics.
Activity restrictions following thyroid biopsies are generally minimal, with most patients able to return to normal activities within hours of the procedure. Avoiding strenuous physical activity or heavy lifting for 24-48 hours helps minimise bleeding risk and reduces strain on the biopsy site. Gentle neck movements and normal daily activities are encouraged to prevent stiffness and maintain normal function. Signs requiring immediate medical attention include excessive bleeding, severe swelling, signs of infection, or pain that worsens rather than improves over time. Most patients find that any initial discomfort resolves completely within 2-3 days, with the biopsy site returning to normal sensitivity and function.