Adenosine cardiac stress testing represents a cornerstone diagnostic tool in modern cardiology, offering physicians critical insights into coronary blood flow when traditional exercise testing proves unsuitable. This pharmacological approach simulates the cardiovascular demands of physical exertion through controlled vasodilation, enabling comprehensive assessment of myocardial perfusion patterns. The procedure has revolutionised cardiac diagnostics for patients with mobility limitations, severe arthritis, or those unable to achieve target heart rates through conventional exercise protocols.
Understanding what occurs during an adenosine stress test empowers patients to approach the procedure with confidence whilst ensuring optimal preparation and cooperation. The test’s sophisticated methodology combines advanced pharmacology with cutting-edge imaging technology, creating a detailed map of cardiac function that guides treatment decisions and risk stratification.
Pre-test preparation and patient assessment protocols
Comprehensive pre-test preparation forms the foundation of successful adenosine stress testing, requiring meticulous attention to patient history, current medications, and physiological status. The preparation phase typically begins 24-48 hours before the scheduled procedure, with specific instructions tailored to individual patient circumstances and medical history.
Contraindications screening for adenosine administration
Medical professionals conduct thorough screening to identify absolute and relative contraindications before adenosine administration. Severe bronchospastic disease, including poorly controlled asthma, represents the most significant contraindication due to adenosine’s potential to trigger bronchospasm through A2B receptor activation. Patients with second or third-degree atrioventricular block without functioning pacemakers require careful evaluation, as adenosine can temporarily worsen conduction abnormalities.
Systemic hypotension, severe carotid stenosis, and known hypersensitivity to adenosine or its components constitute additional contraindications. Recent consumption of dipyridamole-containing medications requires postponement, as these agents can potentiate adenosine’s effects unpredictably. Clinical assessment must also consider unstable angina or recent myocardial infarction , conditions that may increase procedural risk.
Medication withdrawal guidelines including caffeine and theophylline
Caffeine withdrawal represents perhaps the most critical aspect of pre-test preparation, as methylxanthines directly antagonise adenosine receptors. Patients must abstain from all caffeine-containing substances for 24 hours minimum, including coffee, tea, chocolate, soft drinks, and energy drinks. Even decaffeinated products contain trace caffeine amounts and require avoidance during this period.
Theophylline-containing medications demand particular attention, with discontinuation recommended 48 hours before testing. Common theophylline preparations include aminophylline, theophylline sustained-release formulations, and some combination respiratory medications. Over-the-counter preparations containing caffeine, such as certain pain relievers and cold medications, must also be identified and withheld .
Baseline ECG and vital signs documentation
Baseline electrocardiogram recording establishes the patient’s normal cardiac rhythm and identifies any pre-existing conduction abnormalities. A comprehensive 12-lead ECG captures baseline ST-segment morphology, QT interval duration, and any evidence of previous myocardial infarction or ventricular conduction delays. These baseline measurements prove invaluable for comparison during adenosine infusion.
Vital sign documentation includes blood pressure measurements in both arms, heart rate assessment, oxygen saturation levels, and respiratory rate. Temperature recording helps identify any acute illness that might influence test interpretation or patient safety. Some centres perform baseline echocardiography to assess ventricular function and identify structural abnormalities.
Patient consent process and risk communication
Informed consent discussions must thoroughly address the procedure’s purpose, methodology, potential risks, and alternative diagnostic options. Patients require clear explanations of adenosine’s physiological effects, including the temporary nature of symptoms and the rapid resolution following infusion cessation. Risk communication should quantify the likelihood of adverse events whilst contextualising these risks within the broader diagnostic benefit.
Discussion of alternative testing modalities, including exercise stress testing, dobutamine stress echocardiography, or coronary angiography, helps patients understand their diagnostic options. Detailed explanation of post-test monitoring and discharge criteria ensures patients understand the complete procedural timeline .
Adenosine pharmacology and cardiac stress induction mechanisms
Adenosine’s pharmacological profile makes it uniquely suited for cardiac stress testing, with its rapid onset, short duration, and predictable cardiovascular effects. The drug’s mechanism of action involves multiple adenosine receptor subtypes, each contributing to the overall haemodynamic response that simulates exercise-induced coronary hyperaemia.
A1 and A2A receptor activation pathways
Adenosine exerts its cardiovascular effects primarily through A1 and A2A receptor activation, each subtype producing distinct physiological responses. A1 receptor stimulation occurs predominantly in the atrioventricular node, causing negative chronotropic and dromotropic effects that can manifest as transient bradycardia or conduction delays. This mechanism explains the temporary heart rhythm changes commonly observed during adenosine infusion.
A2A receptors, abundant in coronary arterial smooth muscle, mediate the profound vasodilation that forms the test’s therapeutic foundation. Activation of these receptors triggers cyclic adenosine monophosphate elevation, leading to smooth muscle relaxation and coronary artery diameter increases of up to 300-400% above baseline levels.
Coronary vasodilation and steal phenomenon principles
The steal phenomenon represents adenosine’s fundamental diagnostic principle, where maximal vasodilation of normal coronary arteries reduces perfusion pressure to territories supplied by stenotic vessels. In healthy coronary segments, adenosine produces four to five-fold increases in blood flow, whilst stenotic arteries reach their vasodilatory capacity at lower flow rates.
This differential response creates relative hypoperfusion in territories beyond significant stenoses, appearing as perfusion defects on nuclear imaging. The steal effect proves particularly pronounced when stenosis severity exceeds 70% luminal diameter reduction , providing the test’s diagnostic sensitivity for detecting functionally significant coronary disease.
Half-life characteristics and rapid metabolism profile
Adenosine’s extremely short half-life of less than 10 seconds results from rapid cellular uptake and enzymatic degradation by adenosine deaminase and adenosine kinase. This rapid clearance means that adenosine concentrations fall to negligible levels within 30-60 seconds after infusion cessation, explaining the prompt resolution of symptoms experienced by most patients.
The drug’s metabolism occurs primarily within red blood cells and vascular endothelium, with degradation products including inosine, hypoxanthine, and eventually uric acid. This rapid turnover necessitates continuous infusion rather than bolus administration to maintain therapeutic levels during the imaging acquisition period.
Dosage protocols and Weight-Based calculations
Standard adenosine protocols utilise weight-based dosing, typically 140 micrograms per kilogram per minute for six minutes, with tracer injection occurring at the midpoint. Some centres employ abbreviated five-minute protocols, which demonstrate equivalent diagnostic accuracy whilst reducing patient discomfort duration. The infusion rate requires precise calculation based on patient weight, with most protocols targeting plasma adenosine concentrations of 50-100 micromolar.
Alternative protocols may incorporate exercise augmentation, where patients perform low-level exercise during adenosine infusion to improve image quality and reduce side effects. Exercise-augmented protocols typically reduce adenosine dosing to 100-120 micrograms per kilogram per minute whilst maintaining diagnostic efficacy.
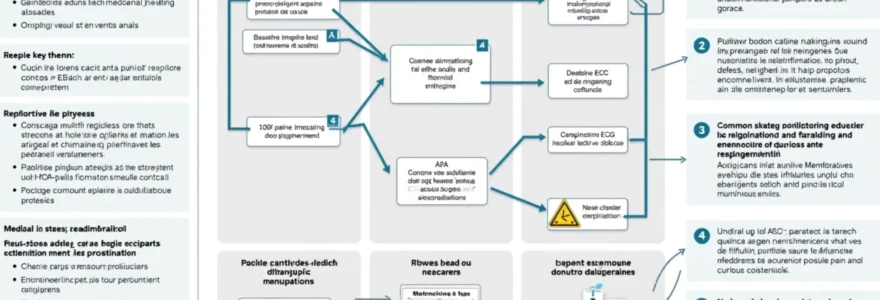
Step-by-step adenosine infusion protocol
The adenosine infusion protocol follows a standardised sequence designed to maximise diagnostic yield whilst ensuring patient safety throughout the procedure. The protocol typically spans 30-45 minutes from initial preparation to completion of tracer injection, with continuous monitoring throughout this period. Initial preparation involves establishing reliable intravenous access, preferably through a large-bore cannula in the antecubital fossa to ensure consistent drug delivery without infiltration concerns.
Patient positioning requires supine placement with slight head elevation for comfort whilst maintaining optimal ECG electrode contact. The infusion pump setup involves precise calculation of adenosine concentration and flow rate based on patient weight, with double-checking procedures to prevent dosing errors. Emergency medications, particularly aminophylline, must be immediately available for rapid reversal if severe adverse reactions occur.
The six-minute infusion protocol begins with gradual adenosine administration at the calculated rate, with symptoms typically appearing within 60-90 seconds of initiation. Radiotracer injection occurs at the three to four-minute mark when maximal coronary vasodilation has been achieved. The infusion continues for an additional two minutes post-tracer injection to ensure adequate tracer distribution to all myocardial territories. Patient communication throughout the procedure helps identify symptom development and provides reassurance about the temporary nature of any discomfort experienced.
Real-time monitoring during adenosine administration
Comprehensive monitoring during adenosine administration ensures immediate detection of adverse events whilst documenting the haemodynamic response necessary for test validation. The monitoring protocol encompasses multiple physiological parameters, each requiring specific attention and predetermined response thresholds for intervention.
12-lead ECG monitoring and arrhythmia detection
Continuous 12-lead electrocardiographic monitoring captures the complete spectrum of adenosine’s electrophysiological effects, from subtle conduction delays to more pronounced arrhythmias. First-degree atrioventricular block commonly occurs, manifesting as progressive PR interval prolongation that typically reverses spontaneously. Second-degree block, particularly Mobitz type I, may develop in susceptible individuals but rarely requires intervention given adenosine’s short half-life.
ST-segment monitoring provides critical safety information, as significant ST depression or elevation may indicate excessive ischaemia requiring immediate infusion cessation. Ventricular ectopy increase during adenosine infusion often reflects the drug’s direct electrophysiological effects rather than ischaemia , though sustained ventricular arrhythmias warrant prompt attention and possible aminophylline administration.
Blood pressure response patterns and hypotensive episodes
Blood pressure monitoring reveals adenosine’s complex haemodynamic effects, typically characterised by modest systolic pressure reduction and variable diastolic responses. Most patients experience 10-20 mmHg decreases in systolic pressure, reflecting peripheral vasodilation and reduced afterload. Diastolic pressure changes prove more variable, sometimes increasing due to compensatory sympathetic activation despite overall vasodilation.
Severe hypotension, defined as systolic pressure below 90 mmHg or greater than 30% reduction from baseline, occurs in approximately 5-10% of patients and may require infusion modification or cessation. Hypotensive episodes typically resolve within 2-3 minutes of adenosine discontinuation , though aminophylline administration may accelerate recovery in severe cases.
Oxygen saturation monitoring and respiratory assessment
Pulse oximetry monitoring detects respiratory complications, particularly important in patients with underlying pulmonary disease. Adenosine can cause bronchospasm through A2B receptor activation, leading to oxygen desaturation and respiratory distress. Baseline oxygen saturation establishment helps identify significant changes during infusion, with desaturation below 90% typically warranting immediate attention.
Respiratory rate monitoring complements oxygen saturation data, as tachypnoea often precedes measurable desaturation. Patients with known respiratory disease require particularly vigilant monitoring, with bronchodilator medications immediately available. Some centres pre-treat asthmatic patients with bronchodilators to minimise adenosine-induced respiratory complications .
Nuclear imaging acquisition timing and technetium-99m protocols
Radiotracer injection timing proves critical for optimal image quality, with most protocols specifying injection at peak adenosine effect, typically 3-4 minutes into the infusion. Technetium-99m-based tracers, including sestamibi and tetrofosmin, require specific handling and injection techniques to ensure adequate myocardial uptake. The tracer dose, typically 20-30 mCi, must be injected rapidly through the established intravenous line to minimise dilution effects.
Post-injection positioning may involve brief low-level exercise to improve tracer distribution and image quality, though this requires careful monitoring given ongoing adenosine effects. Some protocols incorporate immediate post-stress imaging to capture peak perfusion patterns before redistribution occurs . The timing between tracer injection and image acquisition varies by tracer type and institutional protocols, typically ranging from 15-60 minutes post-injection.
Common side effects and emergency management procedures
Adenosine stress testing produces predictable side effects in approximately 80% of patients, most of which are mild, transient, and resolve spontaneously within minutes of infusion cessation. Understanding the expected symptom profile and appropriate management strategies ensures optimal patient care whilst maintaining procedural safety standards.
Chest pain and dyspnoea management strategies
Chest discomfort represents the most commonly reported symptom during adenosine infusion, occurring in 50-70% of patients and typically described as chest tightness, pressure, or burning sensations. This discomfort usually results from direct cardiac effects rather than ischaemia, though differentiation between drug effect and true ischaemia requires careful clinical assessment. Patient education about expected sensations before the procedure significantly reduces anxiety and improves cooperation.
Dyspnoea affects 30-50% of patients, ranging from mild breathlessness to more pronounced respiratory distress. Most dyspnoeic episodes reflect adenosine’s direct respiratory centre effects rather than bronchospasm , though patients with underlying pulmonary disease require careful assessment. Management strategies include reassurance, supplemental oxygen if indicated, and aminophylline administration for severe or persistent symptoms.
AV block recognition and aminophylline reversal protocols
Atrioventricular conduction disturbances occur frequently during adenosine infusion, with first-degree block affecting 10-15% of patients and higher-grade blocks occurring less commonly. Second-degree AV block, when it occurs, typically follows Wenckebach patterns and resolves spontaneously within 1-2 minutes of infusion cessation. Third-degree block remains rare but requires immediate adenosine discontinuation and consideration of aminophylline administration.
Aminophylline protocols typically specify 75-125 mg intravenous doses for severe or persistent conduction abnormalities, though most episodes resolve before intervention becomes necessary. The decision to administer aminophylline should consider symptom severity, haemodynamic stability, and expected spontaneous recovery time . Emergency pacing equipment should remain immediately available, though its use is exceedingly rare in adenosine stress testing.
Bronchospasm prevention in asthmatic patients
Bronchospasm represents the most serious potential complication of adenosine stress testing, particularly in patients with reactive airway disease. Prevention strategies include thorough pre-test screening, consideration of alternative stress agents for severe asthmatics, and prophylactic bronchodilator administration when adenosine use is deemed necessary. Some centres routinely pre-treat asthmatic patients with inhaled beta-agonists 15-30 minutes before adenosine administration.
Recognition of early bronchospastic symptoms enables prompt intervention before severe respiratory compromise develops. Initial management includes immediate adenosine cessation, supplemental oxygen, and nebulised bronchodilator therapy. Severe bronchospasm may require systemic corticosteroids and intensive respiratory support , though such severe reactions remain uncommon with proper patient selection and monitoring.
Flushing and metallic taste symptom duration
Facial flushing affects 20-30% of patients during adenosine infusion, typically appearing within 2-3 minutes of infusion initiation and resolving within 5-10 minutes of cessation. The flushing results from peripheral vasodilation and proves harmless, though patients may find it uncomfortable or concerning without prior explanation. Metallic taste sensations occur in 10-20% of patients and similarly resolve rapidly after infusion completion.
These symptoms require no specific management beyond patient reassurance and monitoring for more significant adverse effects. Documentation of symptom onset and resolution helps establish normal response patterns and guides future testing decisions . Patient education about these expected effects significantly improves tolerance an
d reduces patient anxiety regarding expected sensations.
Post-test recovery and results interpretation timeline
The post-adenosine recovery period requires structured monitoring protocols to ensure patient safety whilst facilitating efficient throughput in busy cardiac imaging departments. Most patients experience rapid symptom resolution within 2-5 minutes of infusion cessation, though individual recovery patterns may vary based on baseline health status and adenosine sensitivity. The recovery phase encompasses vital sign normalisation, symptom assessment, and preparation for subsequent imaging procedures.
Initial post-infusion monitoring focuses on cardiovascular stability, with blood pressure and heart rate measurements every 2-3 minutes until baseline values return. Most haemodynamic parameters normalise within 5-10 minutes, though some patients may experience prolonged mild hypotension requiring extended observation. Respiratory assessment remains important, particularly for patients who experienced dyspnoea during infusion, with pulse oximetry monitoring until oxygen saturation stabilises above 95%.
Patient mobilisation typically occurs once vital signs stabilise and symptoms resolve completely, usually within 10-15 minutes post-infusion. Some centres require a brief observation period before discharge, particularly for patients who experienced significant side effects or required aminophylline administration. Documentation of recovery timeline and symptom resolution provides valuable information for future stress testing decisions. Clear discharge instructions should address activity restrictions, symptom monitoring, and when to seek medical attention if concerns arise.
Results interpretation follows a systematic timeline that begins with immediate safety assessment and progresses through comprehensive image analysis and clinical correlation. Initial image acquisition typically occurs 15-60 minutes post-tracer injection, depending on the specific radiopharmaceutical used and institutional protocols. The nuclear medicine technologist performs preliminary image review to ensure adequate image quality and tracer distribution before patient discharge.
Preliminary results may be available within 2-4 hours for urgent clinical situations, though comprehensive interpretation typically requires 24-48 hours for optimal accuracy. The interpreting physician compares stress and rest images to identify perfusion defects, assess their extent and severity, and correlate findings with clinical presentation and ECG changes during the procedure. Final reports integrate nuclear imaging findings with haemodynamic responses, symptom development, and any ECG changes observed during adenosine administration.
Risk stratification based on adenosine stress test results follows established guidelines that categorise patients into low, intermediate, or high-risk groups for future cardiac events. Normal perfusion studies in appropriate clinical contexts typically confer excellent prognosis, with annual cardiac event rates below 1% in most patient populations. Abnormal results require correlation with clinical symptoms, ECG findings, and other cardiovascular risk factors to guide subsequent management decisions, which may include medical optimisation, further testing, or referral for invasive coronary evaluation.